Addiction, Depression, Suicide: The Risks Don’t Go Away
It’s doubtful that anyone enters into illicit drug practices with the intention of abusing drugs, let alone becoming addicted. More often than not, the initial decision to experiment or engage in drug-using practices brings on unforeseen consequences. In the process, a person loses the ability to stop using, or at the very least ends up resuming drug use.
During the course of a developing addiction, marked changes take place as the effects of drugs interact with the brain’s chemical environment. With continued drug use, these changes have a compounding effect, reinforcing the drug abuse cycle while creating a state of physical dependency along the way.
After a certain point, the effects of drugs on a person’s emotions come into play, which only works to aggravate drug-using behaviors. Unbeknownst to the addict, occasional symptoms of depression and unease turn into a downward spiral of helplessness that can lead to deadly ends.
Addiction’s Effects on Brain Chemistry
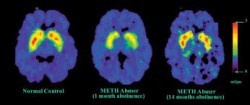
Addiction can have a massive impact on brain functioning.
Addictive substances, such as alcohol, opiates, and stimulants all produce psychoactive effects, altering brain chemical processes in harmful ways. According to California State University, psychoactive agents act on certain key cells throughout the brain and central nervous system, forcing the release of neurotransmitter chemicals.
Neurotransmitters, such as dopamine, GABA, serotonin, glutamate and norepinephrine play integral roles in regulating most all of the body’s major systems. Any disruption or interference in neurotransmitter production rates can cause serious problems to a person’s physical and psychological health.
Over time, brain chemical processes come to rely on drug and alcohol effects. At this point, addictive substances have become an integral part of the brain’s overall chemical system.
Addiction’s Psychological Effects
Psychoactive substances have pronounced effects on the brain’s reward system functions. For the most part, the reward system determines what activities or experiences take priority in a person’s day-to-day life. This system draws upon learning, memory and emotion-based processes in the brain and in turn, influences a person’s thoughts, belief systems and overall motivations within any given day.
According to Indiana University at Bloomington, what most distinguishes addictive substances is their ability to become a major focus in a person’s life regardless of any negative consequences that result. What starts out as a recreational pursuit morphs into a daily obsession that’s pursued at the expense of other important areas of a person’s life.
Addiction & Psychological Dysfunction
Psychological dysfunction develops out of a state of ongoing chemical imbalance in the brain. Since neurotransmitter outputs of dopamine, norepinephrine and serotonin determine a person’s emotional state from one moment to the next, ongoing disruptions in chemical outputs place a person at risk of developing psychological disorders.
According to the Medical University of South Carolina, an estimated 50 percent of drug addicts and 40 percent of alcoholics develop psychological disorders as a result of the effects of drugs and alcohol on brain chemical functions. Psychological disorders most often associated with substance-based addictions include:
- Depression-based disorders
- Anxiety-based disorders
- Personality disorders
- Schizophrenia
In effect, addiction and mental illness both function as brain diseases, so the presence of one condition increases the risks of developing the other.
Addiction’s Links to Depression
Physical Dependency
Frequent drug (or alcohol use) causes considerable damage to brain cell structures as well as brain cell functions. With each drug dose, brain cells work harder than normal to produce large amounts of neurotransmitter chemicals. These activities place a strain on cell structures, which inevitably start to deteriorate from overuse. As cell structures deteriorate, the brain becomes more dependent on drug effects to produce needed chemical supplies.
With an overabundance of neurotransmitter chemicals present, the brain employs an “auto-adjust” mechanism that works to reduce its own natural secretion processes in an effort to conserve chemical supplies. The effects of deteriorating brain cell structures combined with the brain’s “auto-adjust” response creates a state of physical dependency on drug effects.
Withdrawal Effects
The physical dependency brought on by frequent drug use opens the door for depression symptoms to take root. Withdrawal effects develop when needed amounts of a drug are lacking. While different types of drugs tend to produce different types of withdrawal effects, depression-type withdrawal symptoms develop regardless of the type of drug used.
When withdrawal effects take shape, addicts take more of the drug to gain relief from uncomfortable withdrawal symptoms. In effect, withdrawal effects act as a type of negative reinforcement, driving ongoing drug use.
Tolerance Level Increases
The longer a person keeps using drugs or alcohol, the more severe withdrawal effects become. This can have grave implications as far as depression symptoms go.
On top of physical dependency and withdrawal, the damage done to brain cell structures makes them less responsive to a drug’s effects. When this happens, the brain’s tolerance for the drug increases. Increasing tolerance levels drive users to increase dosage amounts to compensate for weakened brain cell functions, otherwise the drug’s desired effects cannot be felt.
Tolerance level increases continue for as long as a person keeps using drugs. This means depression symptoms will become progressively worse in the process.
Suicide Potential
According to the Substance Abuse & Mental Health Services Administration, the likelihood of attempting suicide is 6.2 times greater for people affected by drug and alcohol addiction. In 2005, drug-related suicide attempts accounted for 132,500 emergency room admissions.
In cases where a person struggles with both addiction and depression, these two conditions feed into one another with symptoms of one condition aggravating symptoms of the other. Addicts experiencing depression will likely use drugs in an attempt to self-medicate uncomfortable symptoms. In turn, the effects of continued drug use on brain chemical functions only works to increase the frequency and severity of depression symptoms.
Addiction: A Never-Ending Cycle
The combined effects of withdrawal and increasing tolerance levels keeps the cycle of drug abuse in motion. The resulting effects of drugs on brain reward system functions create a psychological dependency, which underlies and drives the addiction cycle.
The abuse/addiction cycle naturally breeds depression symptoms as brain chemical imbalances worsen over time. Likewise, depression symptoms worsen in severity with continued use, so the risk of developing suicidal ideations increases accordingly. Unless a person seeks out needed treatment help, these risks won’t go away.
